
GET TO KNOW THYROID CANCER
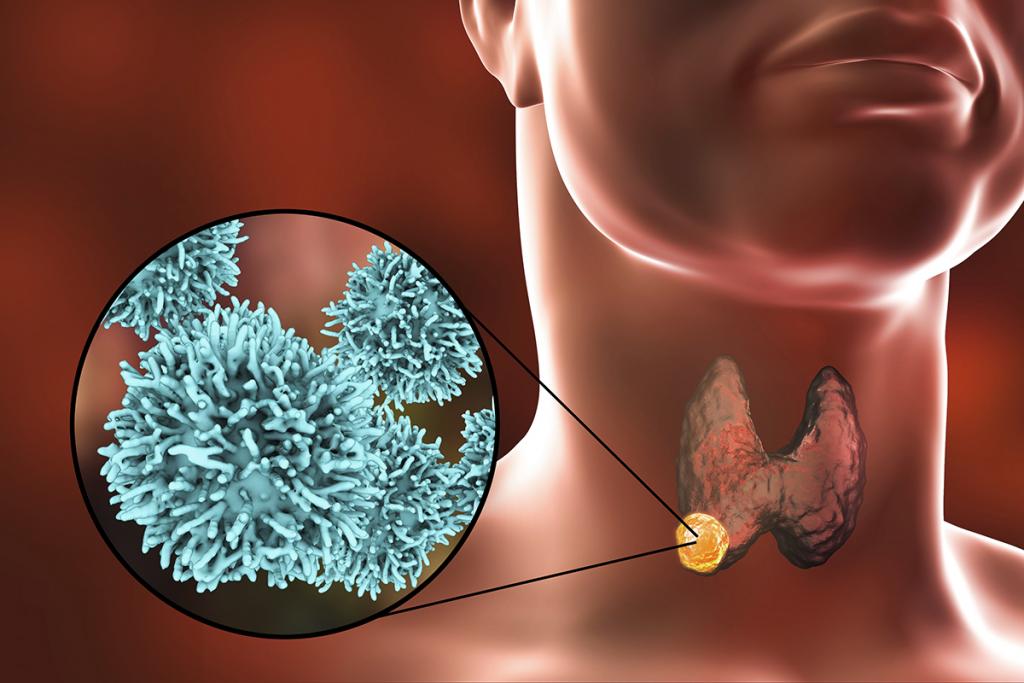
The thyroid gland is a butterfly-shaped organ located at the front of the neck, below the Adam’s apple. Thyroid gland produces hormones acting throughout the body, influencing metabolism, growth and development. Thyroid nodules are solid or fluid-filled lumps that form within the thyroid gland. They can be both non-cancerous and cancerous nodules. These nodules usually grow larger and they can be noticed as a single nodule or multiple nodules in a diffusely enlarged thyroid. Uniquely, the thyroid nodules move during swallowing. Most of thyroid nodules have been accidentally detected during other head and neck investigations. Thyroid cancer occurs when cells undergo genetic changes or mutations. The mutations allow the cells to grow and multiply rapidly and uncontrollably. These cells lose the ability to die and the accumulating abnormal thyroid cells form a tumor. The cancerous cells can further invade nearby tissue and they can spread to other parts of the body. Recently, the incidence of thyroid cancer has increased dramatically during the last 2-3 years present with increased numbers of new cases every year.
Warning signs and symptoms
Thyroid cancer might not exhibit any symptoms at the beginning. Thyroid gland is located at the front of the neck and it is usually not palpable. Most of thyroid nodules grow slowly over several years and they are usually left undiagnosed or untreated. However, as the nodules grow, they often cause swelling, palpable mass in the neck. If mass or lump is detected or seen especially while swallowing, immediate medical attention must be sought and timely diagnosis must be obtained. Contributing factors to thyroid cancer are:
- Female sex. The incidence of thyroid cancer is significantly higher in women compared with men. However, thyroid masses found men are more likely to be thyroid cancer.
- Thyroid cancer is commonly found in people aged less than 20 or over 70.
- Rapid growth of thyroid nodules.
- Exposure to high levels of radiation.
- Family history of thyroid cancer.
Diagnosis
Physical examination often reveals palpable thyroid mass or lump at the front of the neck. The mass is present with rough and poorly defined or undefined borders. If the mass compresses surrounding organs, it can cause changes to the voice including hoarseness, difficulty breathing or swallowing and pain in the neck and throat. Other tests involve:
- Blood tests: To detect thyroid hormones and thyroid functions.
- Ultrasound imaging: Ultrasound uses high-frequency sound waves to create pictures of the thyroid gland structures. The appearance of thyroid gland shown on the ultrasound helps to identify the amount of thyroid nodule and determine whether detected thyroid nodule is likely to be noncancerous (benign) or whether it might be cancerous.
- Fine needle aspiration biopsy: To identify whether the nodule is cancerous, the thyroid tissue needs to be removed. During a fine-needle aspiration biopsy, the doctor inserts a long, thin needle through the skin and into the thyroid nodule. Ultrasound is typically used to precisely guide the needle to reach the nodule. The needle is then used to remove samples of suspicious thyroid tissue. The sample is further analyzed under microscopic examination for pathological assessment. Fine-needle aspiration biopsy is an efficient and reliable means for the evaluation of thyroid nodules. It has been shown to have a reported diagnostic sensitivity and accuracy of 90%. If thyroid cancer is diagnosed, surgical approach remains primary treatment. Since thyroid cancer gradually grows with good prognosis, most thyroid cancers are very curable if treated appropriately in timely manner.
Treatment
Thyroid cancer is classified into different types based on the cells found in the tumor. The type of thyroid cancer is considered in determining treatment plan and disease prognosis. The major treatment for thyroid cancer is surgery. Type of selected surgery primarily depends on the type and the size of the cancer whether it has spread beyond the thyroid gland. In some cases, radioactive iodine treatment using large doses of radioactive form iodine might be considered after surgery to destroy any remaining healthy thyroid tissue, as well as microscopic areas of thyroid cancer that were not surgically removed. Radiation therapy and chemotherapy are not frequently used to treat the common types of thyroid cancer.
Thyroid surgery
Surgeries that are frequently used to treat thyroid cancer include:
- Thyroidectomy (removing all or most of the thyroid gland): A surgery to remove the thyroid gland might involve removing all of the thyroid tissue (known as total thyroidectomy) or most of the thyroid tissue (known as near-total thyroidectomy).
- Thyroid lobectomy (removing a portion of the thyroid gland): During a thyroid lobectomy, only some part of the thyroid gland is surgically removed. It might be recommended if the patients have a slow-growing thyroid cancer in one part of the thyroid and no suspicious nodules in other areas of the thyroid gland.
- Lymph node dissection (removing lymph nodes in the neck): When removing the thyroid gland, the surgeon might need to remove nearby lymph nodes in the neck if there is a chance of cancer spreading to adjacent lymph nodes.
During the surgery, the surgeon often leaves small rims of thyroid tissue around the parathyroid glands to reduce the risk of damage to the parathyroid glands, which help regulating the calcium levels in the blood and prevent low blood calcium after surgery. There is a risk that the nerves connected to vocal cords might not function normally after surgery, which can cause vocal cord paralysis, hoarseness, voice changes or difficulty breathing. Due to advancements in surgical technique and the expertise of highly specialized surgeons, these related nerves can be preserved during the surgery, resulting in the prevention of vocal cord-related complications.
Prior to surgery, patients will be thoroughly examined to assess their physical conditions and any other medical problems before being anesthetized. Surgery to remove thyroid cancer takes approximately 2 hours or longer, depending on each patient’s condition. After surgery, patients are allowed to eat regular food under close supervision of medical team. A 3-5 day hospital stay is required in order to ensure that postoperative complication does not arise. From there on, patients will be discharged from the hospital and they can get a full recovery at home.
Subsequently, removed thyroid mass will be sent to the pathologist for pathological assessment under microscopic examination. If pathological results potentially indicate that cancerous cells are likely to diffusely spread or metastasize to other organs in the body, radioactive iodine treatment will be additionally prescribed after surgery 4 weeks. During receiving radioactive iodine treatment, patients are required to be hospitalized for 2-4 days. The radioactive iodine as a capsule or liquid is taken up mainly by thyroid cancer cells and it is mostly excreted from the body through urine and feces in the first few days after treatment. Patients will be given instructions for precautions to protect other people from the radiation. Before being discharged, the level of radioactive activity will be measured, ensuring that the level falls within non-biological harm range.
In general, thyroid cancer has favorable prognosis, meaning a good chance of treatment success. In fact, most types of common thyroid cancer are usually treatable and in many cases can be cured completely, especially if the disease is caught at earliest stages. Complications are rarely found if the treatments are given by highly experienced specialists in the certified hospital with international standard of care. In addition, the rate of disease recurrence is fairly low. After treatment, patients are able to return to their daily activities with improved quality of life.