Liver cancer
Overview
For most people conventional wisdom dictates that overconsumption of alcohol can lead to cirrhosis which in turn will lead to liver cancer, while others may mistake the two conditions as one and the same. Today, Thai people consume less alcohol; as such cases of cirrhosis have decreased. However, liver cancer is not only caused by alcohol, your diet can play a major part in the onset of this condition. For example foods containing components of alcohol, when consumed in high amounts can lead to cirrhosis or liver cancer.
The main causes of liver cancer however are Hepatitis B and C (with B more common). In many cases this will be congenital and contracted from the mother in the womb, or it may come from husband-wife, or partner. Hemochromatosis can cause permanent damage and liver failure. Liver cancer may also be linked to obesity and fatty liver disease.
Hepatitis B and C are communicable in the same way as AIDS, however it is considered to be more contagious. Once the virus enters the bloodstream it will make its way to the liver, whether or not this will result in hepatitis will depend on the individual’s immunity (which may vary, for details visit www.loveliver.net). For others, the condition may become chronic and last 10-20 years leading to cirrhosis and the potential for cancer developing cells.
Individuals with Fatty Liver, especially those with diabetes are at risk of cirrhosis. It is recommended that they receive medical consultation and ultrasound diagnosis as well as check-up for liver cancer.
Hepatitis is a major cause of cirrhosis and liver cancer; as such the medical community and wider public are paying more interest in this particular disease. For example, more blood tests are being conducted to diagnose hepatitis, as well as vaccines for hepatitis B. Furthermore, more treatments through medication are becoming readily available.
During a test for hepatitis or liver cirrhosis your doctor will often order a liver cancer diagnosis to be conducted simultaneously. This can be significant as early diagnosis of liver cancer will greatly increases the chances of successful and effectiveness of treatment.
A tumor that is left undiagnosed and allowed to grow may cause symptoms such as pain, tightness in upper right abdomen, reduced appetite, and drastic weight loss. Other symptoms may include issues with digestion, constipation, and lymphoma. Note that these symptoms may indicate liver cirrhosis, and not necessarily cancer.
The best method of cancer treatment is early detection and prevention; as such suspicions of Hepatitis should be met with a prompt check-up.
Screening
Diagnosis is conducted according to risk factors such as chronic hepatitis B and C, family history of liver cancer, detection of lumps, and abnormal blood results.
Screening
Screening is usually conducted through an ultrasound of the abdomen which focuses primarily on the liver. Ultrasound utilizes sound waves to create images and poses no health risks. A blood test can also be used to detect abnormalities, such as AFA (alphafetoprotein) count, this is effective in 40% of liver cancer diagnosis. It is recommended to receive cancer screening twice a year.
Diagnosis

After the ultrasound and blood test (to check AFP levels), further diagnosis will be conducted via CT scan or MRI. These will be able to provide a clearer picture of the size, shape, location, spread, blood circulation, and surrounding organs with regards to the tumor. Importantly, it indicates whether the cancer has spread to the lymph nodes, adrenal gland, lung, and bone. If there are indicators your doctor may order further tests such as an x-ray of the lungs and a bone scan. Furthermore, a biopsy may be conducted to provide confirmation (up to 100%) of cancer.
Treatment
Surgical Treatment
There are several methods of cancer treatment the choice of which will depend on each patient’s condition. Liver cancer is often caused by liver cirrhosis as such a factor in treatment is measuring the severity of cirrhosis as it can cause your body to become weak through malnutrition and may cause poor immune system, issues with blood coagulation, enlarged abdomen, internal bleeding and more. These will also cause limitations on surgical treatment, in fact only 10-20 percent of patients will be suitable for surgery due to factors such as cirrhosis.
Surgical treatment is a good option for individuals who do not have cirrhosis, size of tumor is not extremely large, there is no blockage, and the cancer has not spread outside the liver. With surgery, consideration must be given to sedatives required, recuperation post-surgery, other pre-existing conditions, costs, and the experience and expertise of surgical oncologists.
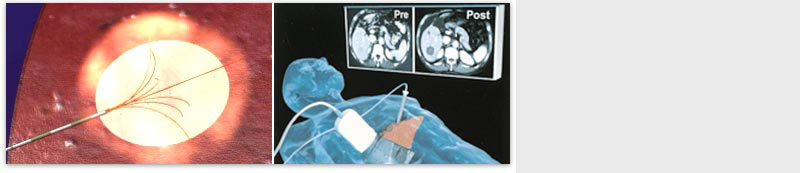
RF Ablation
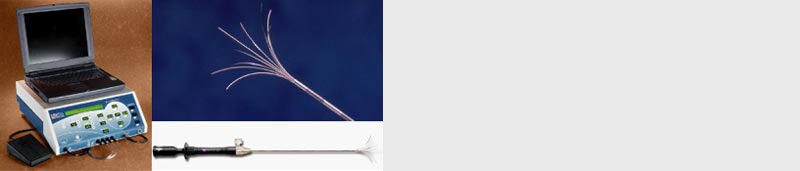
Today, liver cancer and lung cancer are major illnesses for Thai people; this does not include other types of cancers that may have spread to the liver and lungs. Only a small number of patients will be suitable for surgical treatments. Patients who are unsuitable may be due to lack of time needed for successful outcomes of surgery, or being physically unfit for surgery. Luckily in the past 20 years there have been significant developments in the medical community with regards to cancer care. This includes developments in ablation, chemotherapy, and medication. In the past 5 years there have been attempts to develop non-surgical treatments that offer the same benefits as surgery. This includes brachytherapy with the assistance of x-rays and ultrasound. Once the medical device is inserted in the desired position, your doctor may decide to provide other treatment methods such as RF Ablation.
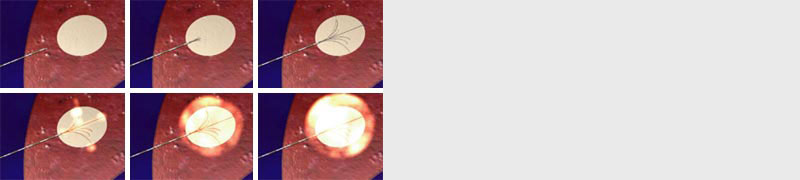
Radiofrequency ablation for cancer is a minimally invasive procedure that uses electrical energy and heat to destroy cancer cells. During radiofrequency ablation for cancer, imaging tests are used to guide a thin needle through the skin or through an incision and into the cancer tissue. High-frequency energy passes through the needle and causes the surrounding tissue to heat up, killing the nearby cells. RF is used for tumors in the liver that are no larger than 4 centimeters, and number less than 4 at a time, it can also be applied to tumors in the lung that are no larger than 3 centimeters. Furthermore, in cases where surgery is preferably avoided RF ablation can be used to treat tumors in the kidney, endocrine gland, and bone.
Advantages of RF include:
- Avoid surgical treatment and as such avoid anesthesia
- Minimally invasive – small scars
- Patients only need to spend 1-2 days in the hospital before being able to return to daily activities
- Less chance of complications compared to surgery
- Reduces chances of bleeding or unnecessary tissue destruction especially in the case of liver tumor
- The chances of hemorrhaging is at 3% (and most will stop by themselves)
- Mostly requires one session, however some cases may require more
- RF ablation is particularly effective in treatment of liver and lung cancer
Liver cancer or tumor often makes it difficult for surgery, as there are numerous complications that may occur such as cirrhosis or hepatitis. Most effective treatments involve insertion of chemotherapy medication intravenously. Presently treatments of tumors smaller than 4-5 centimeters that are inoperable are done through RF ablation.
RF ablation is a treatment that uses imaging guidance to place a needle electrode through the skin into a liver tumor. High-frequency electrical currents are passed through the electrode, creating heat that destroys the cancer cells. At 100 degrees Celsius, the procedure should take approximately 20-40 minutes (depending on size and quantity of tumor). The advantage of RF ablation is that it does not require surgery, and very small amounts of medication such as low quantities of anesthesia. Today it is used to treat liver cancer, or cancers that have spread to the liver, and lung cancer. RF Ablation at Wattanosoth Hospital is provided by specialized radiologist, oncologists, and doctors specialized in Gastroenterology.
Transcatheter Arterial Chemoembolization
For tumors smaller than 4-5 cm surgical treatment may be appropriate (10-20% of patients). If surgical treatment and RF ablation are considered to be ineffective a TOCE may be considered, this refers to transcatheter arterial chemoembolization and involved the use of a catheter.
Guidelines (Preparation)
Patients are recommended to avoid eating at least 4 hours prior to receiving a blood test to determine liver function and coagulation. During treatment an IV catheter, sedatives, and antibiotics may be administered to the patient. Please inform your healthcare provider if you have any medical allergies. Treatment is often painless as such anesthesia is not required, however patients may request painkillers or sleeping pills.
Treatment Method:
The patient will be sent to a hygienic test lab to receive a vascular X-ray. Your doctor will then administer anesthesia through the right groin utilizing a small catheter (less than 2mm. in diameter). The vascular x-ray will be used to navigate the catheter into the liver’s blood vessels. A special substance is then injected which can help to decrease the size of the tumor. Anticoagulants are then administered to reduce the amount of blood (nutrients and oxygen) that are supporting the tumor. Once completed, the catheter will be pulled out and pressure will be applied to the wound for approximately 10 minutes. As the wound is very small it will not require any stitches.
Guidelines after procedure:
Patients will be recommended to remain in bed and extend the leg which received the catheter for a period of 6 hours. Patients will be allowed to eat and drink as long as this does not cause nausea or vomiting. During these 6 hours any urination or defecation will have to occur on the bed, furthermore your nurse will change your bandages the next day. If the patient experiences pain around the catheter entry site or abdominal pain please inform the nurse. Some patients may experience significant nausea; however this can be treated with medication.
Side-effects of treatment:
This method is relatively safe and poses minimal complications. 40% of patients may experience some abdominal tightness and swelling around the catheter entry site. However, most symptoms will subside within a week.
Frequency of Treatment:
On average it takes approximately 2 sessions a month apart. During the second session an x-ray will be performed to determine if alternative treatments such as RF Ablation are required.
Treatment with Radioembolization
Treatment with Radioembolization is a relatively new technique for liver cancer which has spread into the veins. Its principles are similar to TOCE or TACE and involve using a catheter to reach the tumor to inject a radiopharmaceutical referred to as Yttrium which will take effect within a few hours, then dissolve leaving no traces within the patient’s body.
Radioeembolization or SIRT (Selective Internal Radiation Therapy) is considered a relatively expensive procedure due to the cost of pharmaceuticals and equipment imported from abroad. Furthermore, the process if more complicated than TOCE specifically with regards to the injection and side-effects. Side-effects may include abdominal pain, nausea, and vomiting in the 1-2 days after treatment. Although treatment results may be similar to TOCE, this method allows for treatment of cancer which has already spread to the veins.
Author
Dr. Komgrit Tanisaro
Intervention Radiologist